Patient Management on the Platform
Easily perform eligibility checks and manage patient visits.
Step by Step Guide
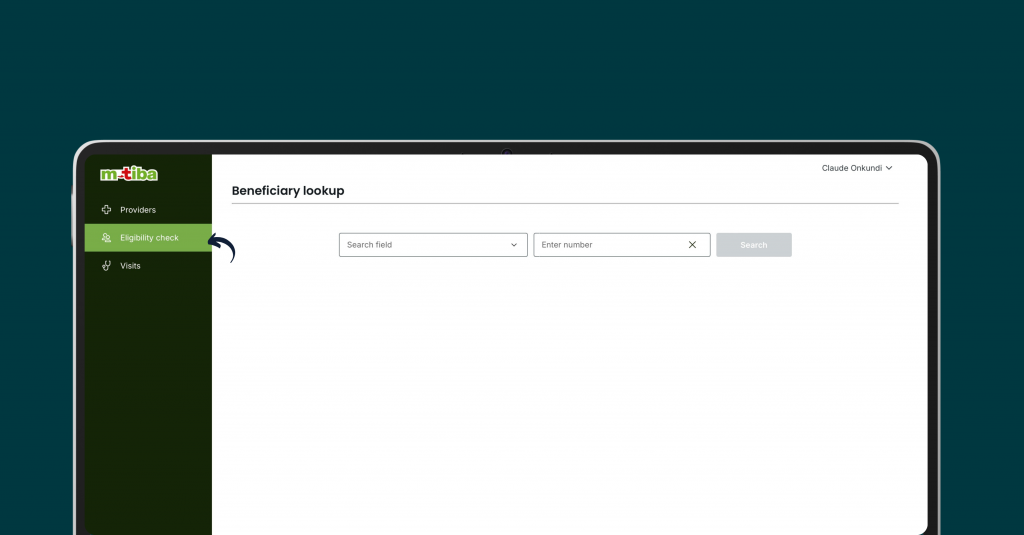
Access the Eligibility Check Module
- Locate and click on the “Eligibility Check” module.
Search for the Beneficiary
- Select the desired search criteria (membership number, mobile number, or national ID).
- Enter the relevant information in the provided field.
- Click “Search.”
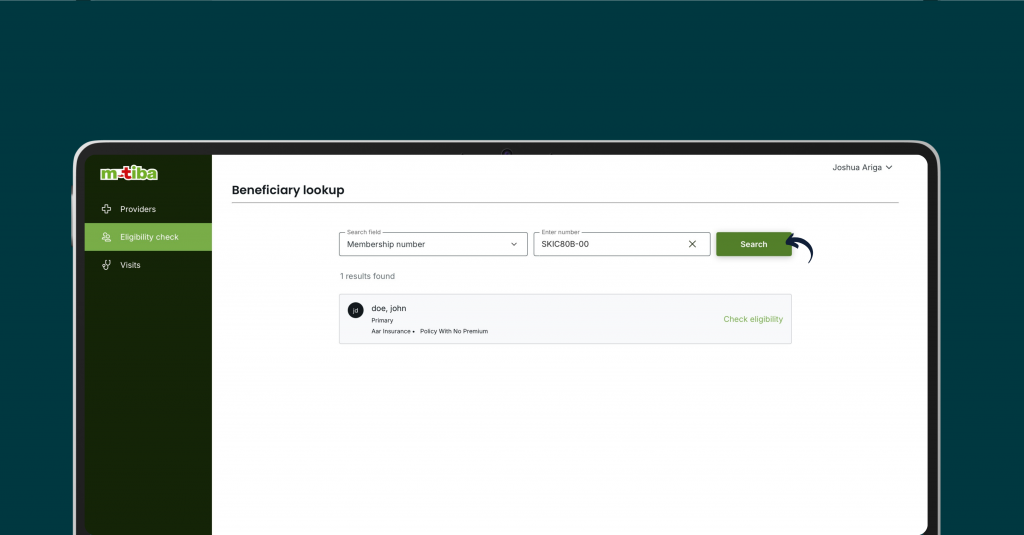
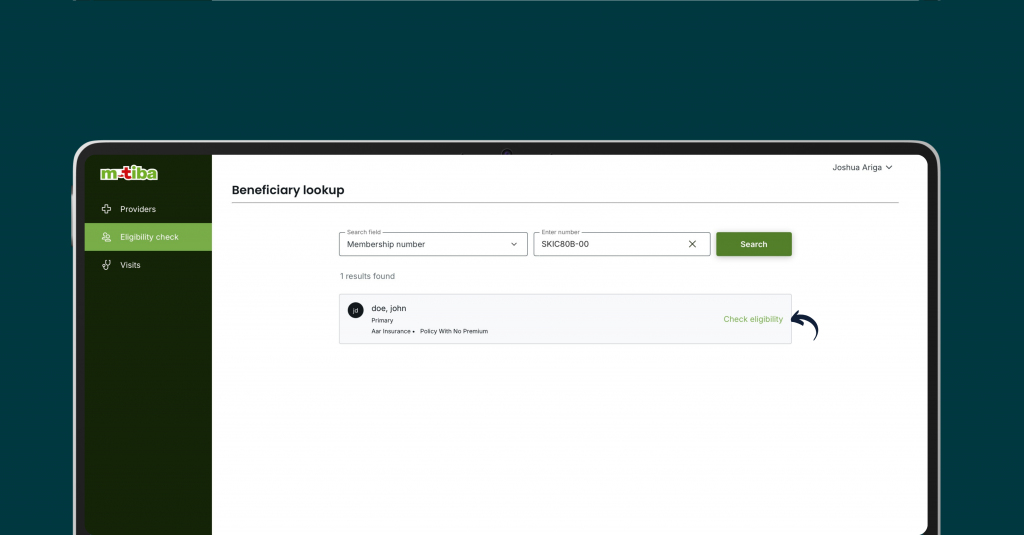
Verify Beneficiary Information
- If the beneficiary is found, verify the displayed details:
- Beneficiary name
- Status or relationship
- Payer name
- Plan
- If the beneficiary is not found, an error message will be displayed.
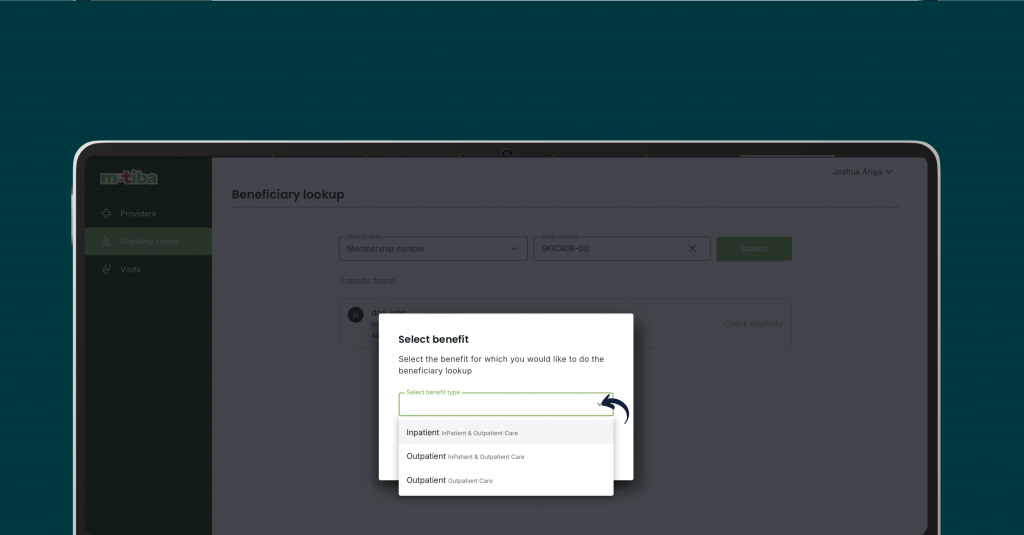
Check Eligibility
- Click the “Check Eligibility” link.
- Select the desired benefit (e.g., inpatient, outpatient).
- Click “Confirm.”
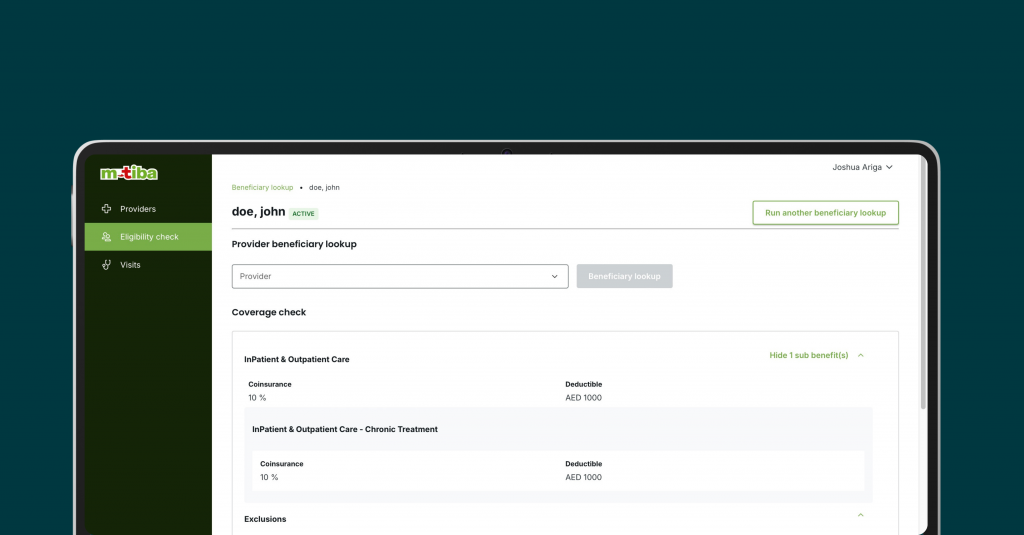
Verify Beneficiary Information
- The beneficiary details page will load, displaying:
- Beneficiary personal information
- Membership information
- Coverage details (coinsurance, deductibles, exclusions)
- Review the information to ensure accuracy.
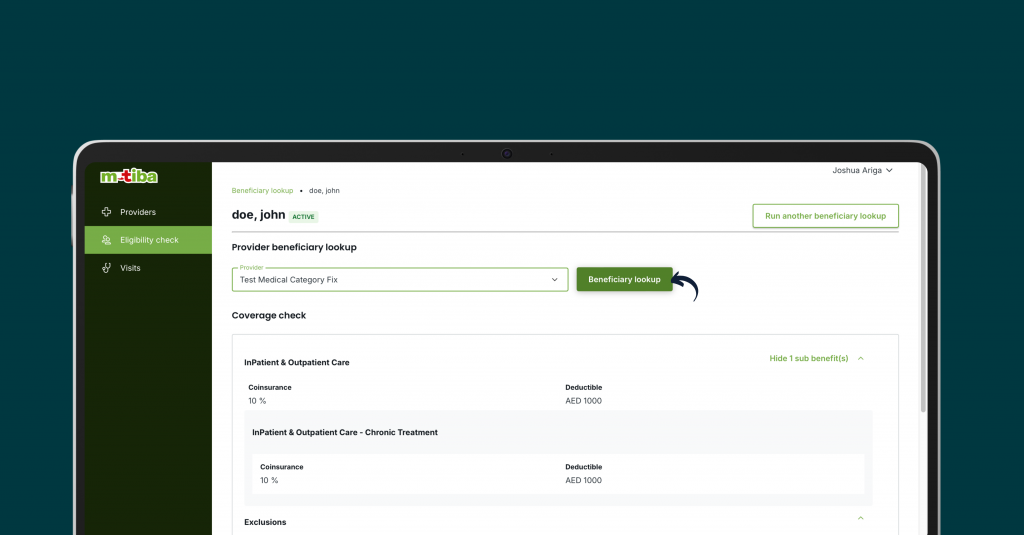
Check Beneficiary Eligibility for a Specific Provider
- Select the desired provider from the dropdown list (if applicable).
- Click “Beneficiary Lookup.”
- A message will indicate if the beneficiary is in-network or out-of-network for the selected provider.
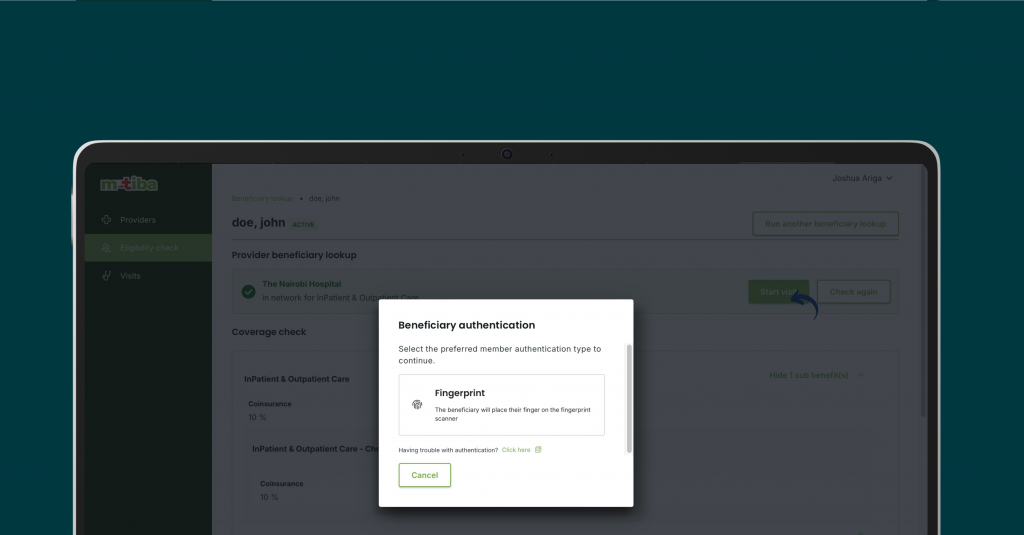
Start Visit (If Eligible)
- If the beneficiary is eligible, click the “Start Visit” button.
- Proceed with the beneficiary authentication process (e.g., fingerprint).
Frequently Asked Questions
You can check a members eligibility by requesting either their:
- Membership number
- Mobile number
- National ID (depending on availability)
- In-network: The member’s plan covers services provided at your facility.
- Out-of-network: The member’s plan may not cover services provided at your facility, or coverage may be limited.
If the system cannot find a matching member, an error message will be displayed. Double-check the entered information and try again. If the issue persists, contact the M-TIBA support team on 0800721253.
Once eligibility is confirmed and the member is in-network, click the “Start Visit” button.
You will be prompted to authenticate the member (e.g., fingerprint).
The beneficiary details page includes:
- Member name
- Date of birth
- Gender
- National ID
- Membership information (payer, plan, policy number, etc.)
- Coverage details (coinsurance, deductibles, exclusions)
- Coinsurance: The percentage of the medical bill that the member is responsible for paying.
- Deductibles: The amount the member must pay out-of-pocket before insurance coverage kicks in.
- Exclusions: Services or conditions not covered by the member’s plan.
- On the eligibility check page, locate the search criteria options.
- Select the desired search criteria (membership number, mobile number, or national ID).
- Enter the required information and click “Search.”
The M-TIBA platform handles administrative tasks and operations related to healthcare plans for insurance companies. This includes processing claims and making payments to healthcare providers on their behalf.