M-TIBA helps insurers launch new markets and segments across Africa—faster, leaner, and with full control. From first pilot to scaled operations, we power growth with the tech and support to get you there.




.png)
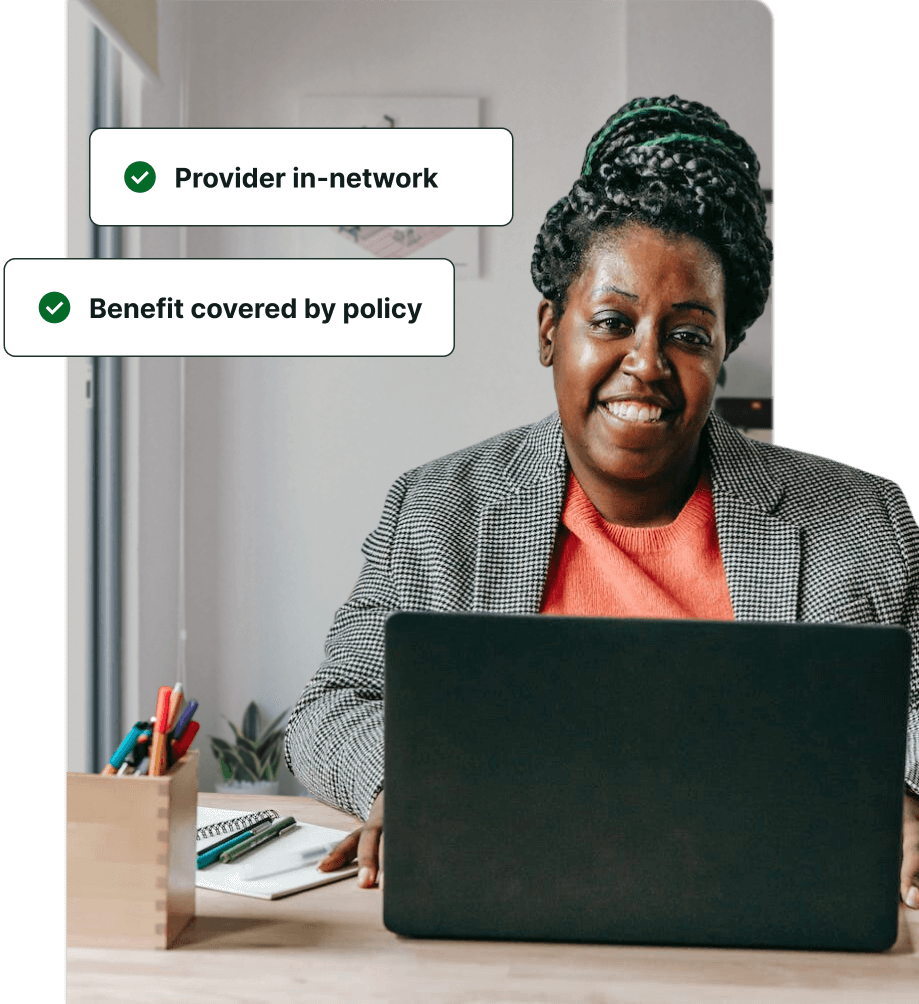
Joy signs up for maternity coverage and is onboarded within minutes. Through the M-TIBA Member App, she instantly checks her benefits and finds a nearby, in-network provider—skipping long waits and guesswork.
The approval process for health insurance takes an average of 7 days in Kenya.

At the maternity clinic, Joy's identity and coverage are quickly verified by the clinic’s receptionist through a digital eligibility check. The receptionist submits a pre-authorization request for Joy through the M-TIBA platform.
M-TIBA reduces the annual admin cost per member from 29 USD to 1 USD.
.jpg)
Using the M-TIBA platform, Joy's Case Manager reviews and approves her pre-authorization request directly. Joy can now get the check-up she needs with the reassurance that the costs are covered by her insurance.
Currently, it takes at least 3 days to process a pre-auth request in Kenya.

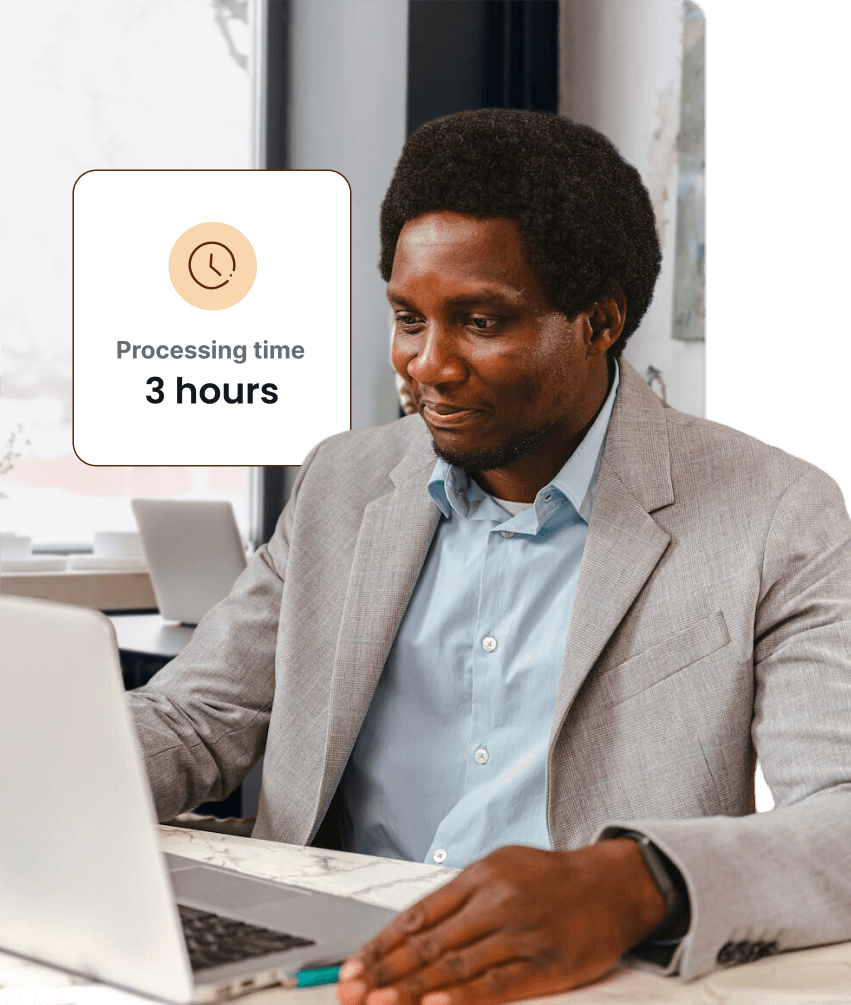
After Joy completes her check-up, the clinic’s cashier submits a claim through the M-TIBA platform. The claim is processed by a Claim Manager within 3 hours, making sure that both Joy and her provider are paid in a timely manner.
Claims submitted in paper form have an average processing time of 30 days.
Thanks to M-TIBA's insights dashboard, Joy’s insurer is able to review their payment forecasts in real-time. Confident that all outgoing payments align with their cash flow, Joy’s payment is approved within 24 hours.
It currently takes an average of 60 days for claims to be paid out in Kenya.

.jpg)
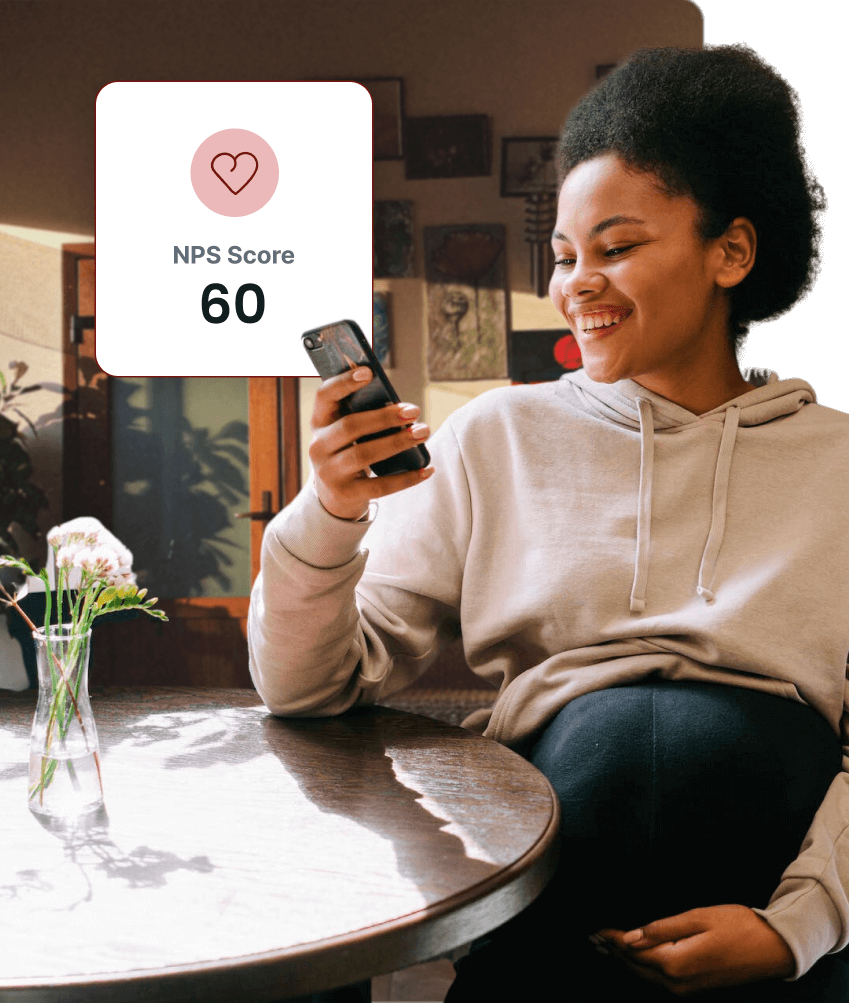
Joy tracks her claim history and benefit usage in real-time through the M-TIBA Member App. After a smooth first experience, Joy finds herself anticipating her future check-ups with increased peace of mind.
M-TIBA has a Net Promoter Score of 60.
.jpg)




.svg)
















