M-TIBA for healthcare providers
Smooth and efficient claims management and billing on M-TIBA
M-TIBA helps you focus on what matters the most – your patients.
- Everything on pre-authorisation
- How to do inpatient and outpatient billing
- Clear overview of claims submission and adjudication
- Helpful tips and information
Simple guide: Care administration and claims processing
Simple guide: Care administration and claims processing
The M-TIBA platform handles administrative tasks and operations related to healthcare plans for insurance companies. This includes processing claims and making payments to healthcare providers on their behalf.
The M-TIBA platform handles administrative tasks and operations related to healthcare plans for insurance companies. This includes processing claims and making payments to healthcare providers on their behalf.
Frequently Asked Questions
M-TIBA streamlines your entire workflow by connecting patients, payers, and providers in one platform. This means:
- Faster patient check-in: Instantly verify insurance, reducing wait times and paperwork.
- Simplified pre authorisation approvals: Submit and track pre-auths electronically.
- Easy claims processing: Submit claims digitally and track them in real-time.
- Faster, reliable payments: Get paid quickly and consistently to improve your cash flow.
By automating tasks and eliminating manual processes, M-TIBA helps you:
- Reduce administrative costs
- See patients faster
- Get paid faster and more reliably
- Focus on delivering quality care to patients
1. Start Treatment:
- Patient: Initiates treatment through USSD (*253#) or through Service Provider portal.
- Service Provider: Opens treatment on the portal under “Create Claim” feature.
2. Patient Information:
- Enter patient’s phone number or membership number.
- Select patient name and program name.
- Choose “OUTPATIENT” as the cover. Verify it’s correct.
3. Member Verification:
- Confirm member validity using biometric verification on M-TIBA system.
4. Claim Details:
- Patient and doctor fill in M-TIBA OP claim form.
- Search for items to bill (e.g., tests, medicines). Enter unit price for each item.
5. Pre-Authorization (if needed):
- Request pre-authorization for services not included in fixed-fee agreement (e.g., MRI).
- Enter doctor’s name and submit request for review.
- Receive pre-authorization confirmation or feedback.
- Bill approved pre-authorization as a claim on M-TIBA.
6. Submit Claim:
- Enter invoice number and diagnosis.
- Add optional comments (e.g., follow-up appointment).
- Attach scans or documents (optional).
- Click “Go to Payment” and then “Pay” buttons.
- Close treatment.
7. Claim Processing:
- M-TIBA Claims Assessor reviews and adjudicates the claim.
8. Payment:
- Approved claims are paid by CarePay to the Service Provider.
- M-TIBA reconciles services billed with fixed-fee
1. Start Treatment:
- Patient: Initiates treatment through USSD (*253#) or through Service Provider portal.
- Service Provider: Opens treatment on the portal under “Create Claim” feature.
2. Patient Information:
- Enter patient’s phone number or membership number.
- Select patient name and program name.
- Choose “DENTAL” or “OPTICAL” as the cover (depending on the service).
3. Member Verification:
- Confirm member validity using biometric verification on M-TIBA system.
4. Claim Details:
- Search for items to bill based on pre-agreed rates (e.g., procedures, materials).
- Enter unit price for each item.
5. Pre-Authorization (always required):
- Request pre-authorization for ALL services.
- Enter details, diagnosis, and submit for review.
- Receive confirmation or feedback on pre-authorization.
- Only bill approved pre-authorization amounts.
6. Submit Claim:
- Enter invoice number and diagnosis.
- Add optional comments.
- Attach scans or documents (optional).
- Click “Go to Payment” and then “Pay” buttons.
- Close treatment.
7. Claim Processing:
- M-TIBA Claims Assessor reviews and adjudicates the claim.
8. Payment:
- Approved claims are paid by CarePay to the Service Provider.
Before Admission:
- Request Pre-Authorization:
- Email scanned M-TIBA pre-authorization form and supporting documents to
care@mtiba.co.ke. - Call M-TIBA call center immediately before admission (toll-free: 0800721253, chargeable:0709071000).
- Email scanned M-TIBA pre-authorization form and supporting documents to
- Await Approval:
- M-TIBA Case Manager reviews your request and confirms if the member can be admitted.
- They may provide further billing instructions.
After Discharge:
- Submit Final Bill:
- Email scanned final itemized bill and discharge summary to
care@mtiba.co.ke.
- Email scanned final itemized bill and discharge summary to
- Receive Confirmation:
- M-TIBA Case Manager confirms the total billable amount.
Open Treatment & Submit Claim:
- Verify Member:
- Use biometric verification on the M-TIBA system.
- Submit Claim:
- Select “IN-PATIENT HOSPITALIZATION” with the correct cover.
- Enter total cost incurred during hospitalization.
- Enter invoice number, diagnosis, and attach scans/documents:
- Pre-authorization form
- Detailed cost breakdown with prices and quantities
- Discharge summary
- Other relevant documents
- Claim Processing:
- M-TIBA Claims Assessor reviews and adjudicates the claim.
- Payment:
- Approved claims are paid by CarePay to the Service Provider.
Important Notes:
- Submit claims within 24 hours of discharge.
- Notify M-TIBA if the bill reaches Ksh. 300,000.
- Ensure invoice amounts on M-TIBA match physical invoices and HMIS.
Claim Accuracy:
- Fill in all fields correctly, especially diagnosis, to avoid rejections.
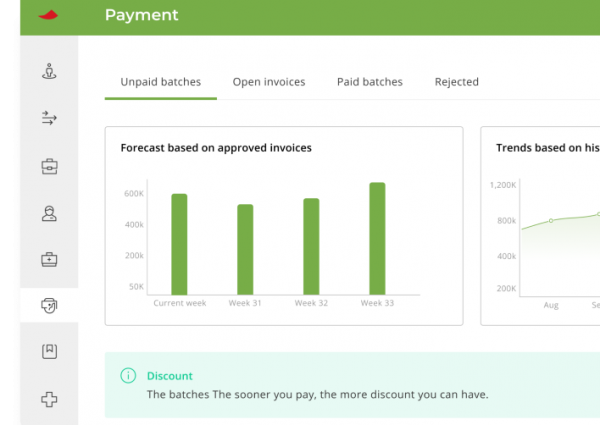
Payment:
- CarePay provides monthly reconciliation reports.
- Payment is based on the number of visits and billed exclusions.
NHIF:
- Scheduled procedures: Request NHIF undertaking for clients. M-TIBA pays the difference after NHIF deductions.
- Emergency procedures: Check if member has NHIF approval. If not, M-TIBA covers the entire cost.
Claims:
- Submit claims within 24 hours of service.
- Fill in the OP claim form electronically (physical copies not required).
- Keep physical forms for 12 months from the treatment date.
- May be requested by M-TIBA Claims Assessors.
M-TIBA streamlines your entire workflow by connecting patients, payers, and providers in one platform. This means:
- Faster patient check-in: Instantly verify insurance, reducing wait times and paperwork.
- Simplified pre authorisation approvals: Submit and track pre-auths electronically.
- Easy claims processing: Submit claims digitally and track them in real-time.
- Faster, reliable payments: Get paid quickly and consistently to improve your cash flow.
By automating tasks and eliminating manual processes, M-TIBA helps you:
- Reduce administrative costs
- See patients faster
- Get paid faster and more reliably
- Focus on delivering quality care to patients
Integrated Providers | These are healthcare providers where M-TIBA has integrated its portal with their HMIS for ease of billing. |
Non- Integrated Providers | These are healthcare providers who bill directly on the MTIBA portal. |
This is dependent on the members insurance cover and the services being sought.
Note: This step-by-step guide applies to both integrated and non-integrated healthcare providers.
Step 1: Send request to email addresses:
For AAR Insurance:
- Send to the 2 email addresses below:
For Jubilee, Fidelity and GA Insurance:
Step 2: Email title:
- [Patient name] / [Scheme] / [Phone number]
Step 3: Attach documents:
- Scanned insurance pre-authorization form
- Any other relevant medical documents
Step 4: Send the request to our Case Manager for approval
Please call us on 0800721253 in case you require further assistance.
Before Admission:
- Request Pre-Auth:
- Send a pre-auth email request to the insurer.
Insurance Company Email Address AAR GA insurance Fidelity MTIBA-Jubilee Pacific - Attach the following documents to your email:
- Completed claims form
- Completed pre-authorization request form
- Diagnostic results (if available)
- Medical reports (if available)
- Send a pre-auth email request to the insurer.
- Wait for Confirmation:
- A Case Manager will review your request and respond via email.
- The email will confirm if the patient is authorized for admission and advise on the appropriate cover for billing.
At Discharge:
- Create a Claim:
- Log in on M-TIBA, create a new claim for the patient.
- Enter the patient’s details accurately and select the correct cover confirmed in the pre-authorization email.
- Verify the patient’s biometrics.
- Bill for Inpatient Stay:
- Create a single line item named “Inpatient Hospitalization” in the claim.
- Enter the total cost of the hospitalization in this line item.
- This will trigger a request for a final pre-authorization for the discharge Letter of Undertaking (LOA).
- Submit Final Pre-Authorization:
- Log in to the M-TIBA system.
- Create a new pre-authorization request with the following details:
- One line item named “IN-PATIENT HOSPITALIZATION” specifying the cover used.
- Total cost of hospitalization to be deducted from the member’s benefit.
- Diagnosis for the hospitalization.
- Attach scanned copies of the following documents:
- Pre-authorization form
- Invoices with detailed breakdown of costs (including prices and quantities)
- Discharge summary
- Any other relevant documents
- Insurer Review and Approval:
- An Case Manager from the insurer will review your pre-authorization request on the M-TIBA system.
- If approved, the Case Manager will attach the discharge Letter of Undertaking (LOA) to the request.
- If not approved, the Case Manager will add comments in the notes section and request additional information from you.
- Final Bill Submission (After Approval):
- Once the pre-authorization is approved, proceed to finalize the bill on the M-TIBA system as agreed with the Case Manager.
- Add an additional line item named “INPATIENT DISCHARGE” with a value of zero Kenya Shillings (Kshs 0).
- Enter the invoice number for the final bill, admission date, and discharge date.
- Submit the final bill.
Inpatient cases | Outpatient cases |
Filled in claims form | Filled in claims form |
Diagnostic results (if applicable) | Medical reports (if applicable) |
Discharge summary | Diagnostic results (if applicable) |
Medical reports (if applicable) |
|
Itemized invoice-at discharge |
|
Requires Preauthorization | Does not require preauthorization |
All admissions and discharges. | KEPI vaccines. |
All day cases. | ANC profiles. |
Advanced imaging e.g. CT scans, MRI etc | Bills of less than KES 15,000 per service point for outpatient. |
General exclusions. | X-rays and ultrasounds |
Bills of more than KES 15,000 per service point for outpatient. | Bills of less than KES 10,000 for dental and optical services.
|
Private vaccines. |
|
Physiotherapy sessions |
|
Drug prescriptions with supplements |
|
Bills of more than KES 10,000 for dental and optical services. |
|
Annual Wellness checks. |
|
Baby friendly vaccines. |
|
- All advanced imaging requests e.g CT scans, MRIs.
- All specialized procedures.
- All advanced lab requests e.g biofire panels.
- In the absence of a fully filled claim form.
- In cases where the diagnosis given does not match the item requested.
- Self-requested examinations.
Bundled services:
All bundled services must be itemized on the claim form e.g packaged lab tests.
1. Start Treatment:
- Patient: Initiates treatment through USSD (*253#) or through Service Provider portal.
- Service Provider: Opens treatment on the portal under “Create Claim” feature.
2. Patient Information:
- Enter patient’s phone number or membership number.
- Select patient name and program name.
- Choose “OUTPATIENT” as the cover. Verify it’s correct.
3. Member Verification:
- Confirm member validity using biometric verification on M-TIBA system.
4. Claim Details:
- Patient and doctor fill in M-TIBA OP claim form.
- Search for items to bill (e.g., tests, medicines). Enter unit price for each item.
5. Pre-Authorization (if needed):
- Request pre-authorization for services not included in fixed-fee agreement (e.g., MRI).
- Enter doctor’s name and submit request for review.
- Receive pre-authorization confirmation or feedback.
- Bill approved pre-authorization as a claim on M-TIBA.
6. Submit Claim:
- Enter invoice number and diagnosis.
- Add optional comments (e.g., follow-up appointment).
- Attach scans or documents (optional).
- Click “Go to Payment” and then “Pay” buttons.
- Close treatment.
7. Claim Processing:
- M-TIBA Claims Assessor reviews and adjudicates the claim.
8. Payment:
- Approved claims are paid by CarePay to the Service Provider.
- M-TIBA reconciles services billed with fixed-fee payment.
1. Start Treatment:
- Patient: Initiates treatment through USSD (*253#) or through Service Provider portal.
- Service Provider: Opens treatment on the portal under “Create Claim” feature.
2. Patient Information:
- Enter patient’s phone number or membership number.
- Select patient name and program name.
- Choose “DENTAL” or “OPTICAL” as the cover (depending on the service).
3. Member Verification:
- Confirm member validity using biometric verification on M-TIBA system.
4. Claim Details:
- Search for items to bill based on pre-agreed rates (e.g., procedures, materials).
- Enter unit price for each item.
5. Pre-Authorization (always required):
- Request pre-authorization for ALL services.
- Enter details, diagnosis, and submit for review.
- Receive confirmation or feedback on pre-authorization.
- Only bill approved pre-authorization amounts.
6. Submit Claim:
- Enter invoice number and diagnosis.
- Add optional comments.
- Attach scans or documents (optional).
- Click “Go to Payment” and then “Pay” buttons.
- Close treatment.
7. Claim Processing:
- M-TIBA Claims Assessor reviews and adjudicates the claim.
8. Payment:
- Approved claims are paid by CarePay to the Service Provider.
Before Admission:
- Request Pre-Auth:
- Send a pre-auth email request to the insurer.
Insurance Company Email Address AAR GA insurance Fidelity MTIBA-Jubilee Pacific - Attach the following documents to your email:
- Send a pre-auth email request to the insurer.
After Discharge:
-
Submit Final Bill:
- Upload scanned final itemized bill, discharge summary, and other supporting documents on the same pre-authorization.
- Ensure the total cost matches the pre-authorized amount.
-
Bill on Approved Pre-Authorization:
- Use the approved pre-authorization to bill the treatment.
- Have the patient verify their biometrics.
- Bill one line item: “Inpatient Hospitalization” with the total cost.
- Attach the following documents:
- Pre-authorization form
- Detailed cost breakdown with prices and quantities
- Discharge summary
-
Claim Processing:
- M-TIBA will review and adjudicate your claim, considering NHIF information if applicable.
- Approved claims will be paid by M-TIBA.
Important Notes:
- Submit claims within 24 hours of discharge.
- Notify M-TIBA if the final bill exceeds the pre-authorized amount through the system.
- Keep physical claim forms for 12 months.
- Ensure invoice amounts on M-TIBA match physical invoices and HMIS.
Claim Accuracy:
- Fill in all fields correctly, especially diagnosis, to avoid rejections.
Payment:
- CarePay provides monthly reconciliation reports.
- Payment is based on the number of visits and billed exclusions.
NHIF:
- Scheduled procedures: Request NHIF undertaking for clients. M-TIBA pays the difference after NHIF deductions.
- Emergency procedures: Check if member has NHIF approval. If not, M-TIBA covers the entire cost.
Claims:
- Submit claims within 24 hours of service.
- Fill in the OP claim form electronically (physical copies not required).
- Keep physical forms for 12 months from the treatment date.
- May be requested by M-TIBA Claims Assessors.